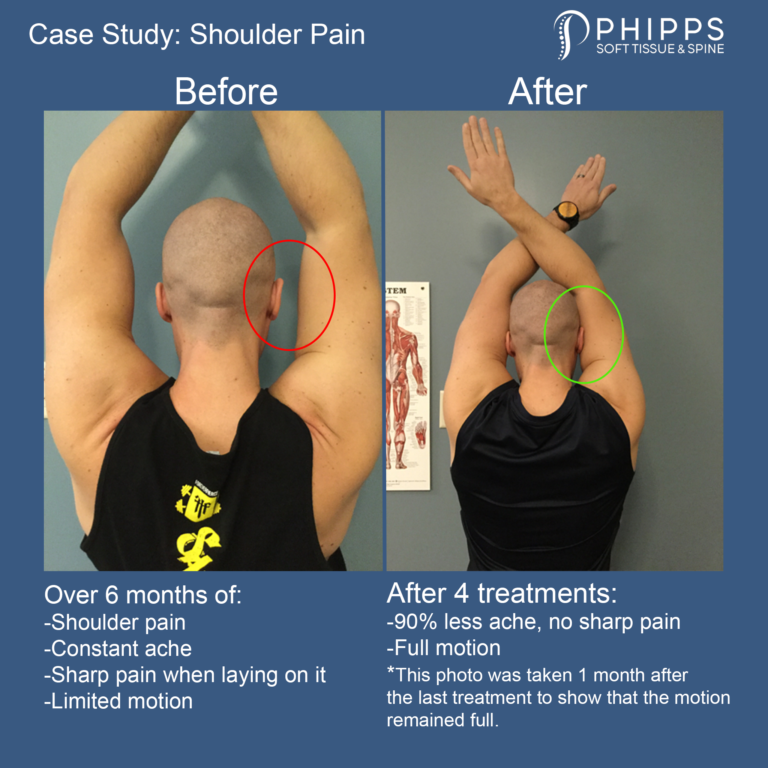
Shoulder Pain: Case Study
Patient: Tim, from Williamsville, NY
History: Right shoulder pain, achy all the time and sharp with certain movements. Pain intensity would get up to a 7 out of 10.
Primary diagnosis: Muscle adhesion in the rotator cuff muscles
Treatment: Manual Adhesion Release™ to the rotator cuff muscles.
Outcome: After 4 treatments, Tim’s shoulder range of motion was fully restored. His shoulder range stayed full even after a month of no treatment. Overall, his symptoms were 90% better after his last visit and are continuing to improve.
To evaluate the health of your shoulders try the mobility assessment outlined below at home.
Passing this mobility screen is crucial to have a pain-free shoulder and prevent injury. If you have shoulder pain or have failed this mobility assessment, then contact us today so we can restore this test and fix your pain.
*Please note that every patient is different. The content and tips displayed on this page are for educational purposes only, and do not substitute for medical advice. Please consult with a medical or healthcare provider, such as Dr. Phipps, for specific diagnosis and treatment advice.
Williamsville, NY 14221 Chiropractor
5 Tips to Make Your Elbow Pain Go Away…and Stay Away

Dr. Phipps is a soft tissue specialist that is an expert at diagnosis and treatment of elbow pain. See some elbow pain treatment and tips* below to help make your elbow pain go away and stay away!
1. If you are experiencing pain in your elbow, it is important to start with an accurate diagnosis from a soft tissue specialist.
Two of the most common causes of elbow pain are adhesion and tendon degeneration:
- Adhesions are the most common cause of pain and stiffness in the elbow and they form from overuse. Learn more about adhesion here.
- Tendon degeneration also occurs from overuse. This is when the tendons of the muscles in your forearm that attach to your elbow degenerate and can result in chronic pain. This can be reversed with the correct treatment and management. But it is important to get the proper treatment as soon as possible as there is a window of opportunity to fix this.
* If you have been labeled with tennis elbow or golfers elbow, you likely have undiagnosed tendon degeneration in your arm that needs specific diagnosis, treatment and management. Schedule a consultation with Dr. Phipps to get started.
2. Avoid ineffective pain treatment methods.
- Stretching, ice, tape, straps, cupping and/or adjustments will not fix adhesion or degenerated tendons. Receiving treatment from a soft tissue specialist is the fastest way to heal elbow pain.
3. Manage the load on your elbow.
- You may need to temporarily reduce activities that make your elbow hurt. Therefore, reducing the stress on the muscle. This needs to be done in conjunction with soft tissue treatment to the muscles and tendons otherwise it is likely your pain will come back.
4. Stop covering up the pain with medication.
- Anti-inflammatories, pain creams, cortisone shots and other types of pain management will not do anything to fix adhesion, or tendon degeneration. In fact, pain medication will make tendon degeneration and adhesion worse and slow down the recovery process.
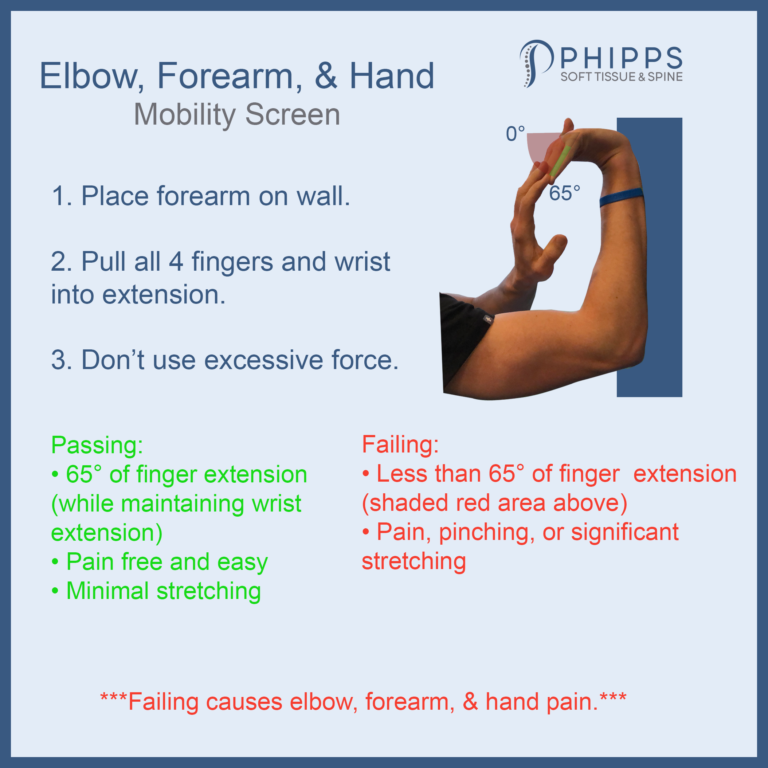
5. Try the elbow mobility self-assessment (see demonstration image below).
- Place your arm against the wall with your elbow at 90°. Use your other had to pull your fingers and wrist into extension. Your fingers should extend about 65° with ease and very little pulling/stretching in your forearm. If you fail this test, you likely have adhesion in the muscles that cause elbow pain.
The earlier you receive the correct treatment for elbow pain, the faster you can get back to living a pain free life. Dr. Phipps is a soft tissue specialist and has special training in the diagnosis and treatment of elbow pain and tennis elbow. Sign up for a 1-on-1 consultation today!
*Please note that every patient is different. The content and tips displayed on this page are for educational purposes only, and do not substitute for medical advice. Please consult with a medical or healthcare provider, such as Dr. Phipps, for specific diagnosis and treatment advice.
Williamsville, NY 14221 Chiropractor
Plantar Fasciitis? Probably Not.
Foot pain is one of the more commonly mismanaged areas of the body. A trip to your family doctor, podiatrist or even to the Internet and you will be labeled with plantar fasciitis. Then, you start icing, stretching, taking anti-inflammatories, rolling your foot with a ball, or may have been convinced that getting a cortisone injection was a good idea. You can continue this routine for months or years with minimal results. Your symptoms may reduce or resolve with time, but only because your body compensated putting extra stress on another area of your body to reduce pressure on your foot. This can lead to pain in your other foot, knee, hip, low-back, and/or reoccurring pain in your injured foot over time.
So, where did you go wrong?
It all starts with an inaccurate diagnosis (plantar fasciitis) that can lead to wrong and ineffective treatment methods. It’s crucial to receive a correct diagnosis and receive the right treatment to stay pain free and continue doing everything you love.
To get an accurate diagnosis regarding your foot, it is best to start with a soft tissue specialist. Click here to contact Phipps Soft Tissue and Spine so you can receive the correct diagnosis and treatment and begin your road to recovery.
Below you will find additional information on foot pain, anatomy, and why plantar fasciitis treatments such as injections, stretching, rolling and ice can be a waste of time.
What exactly is plantar fasciitis?
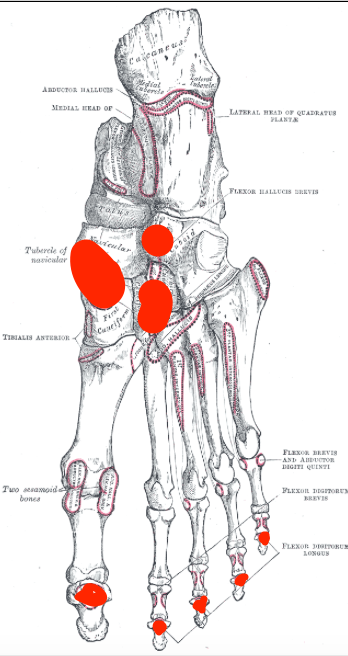
The plantar fascia is a thickened area of connective tissue and is often blamed for pain on the bottom of your foot. The diagnosis of plantar fasciitis implies that the attachment point of the plantar fascia and heel (circled in red below) is inflamed and causing pain.
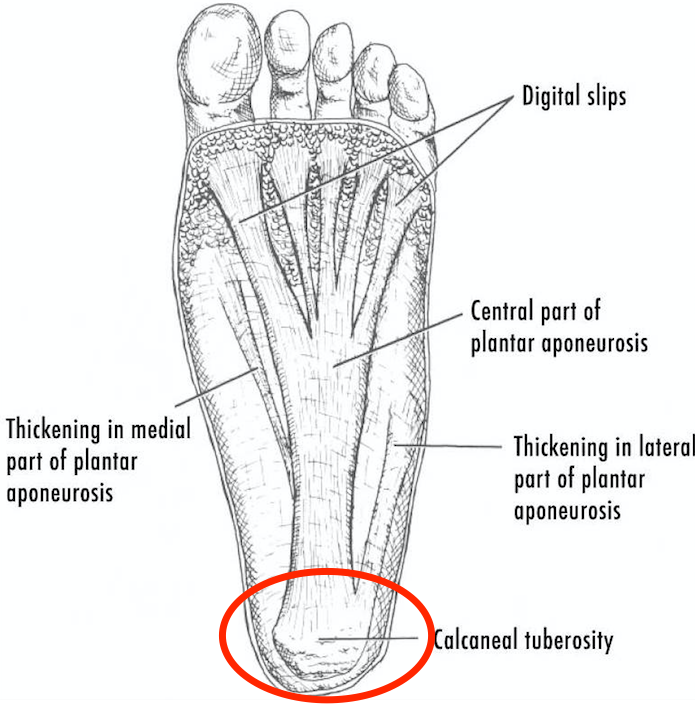
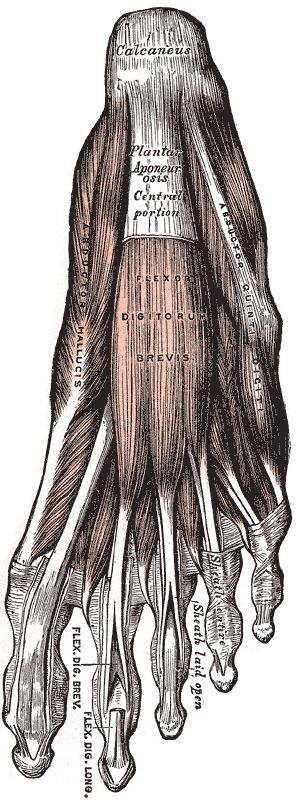
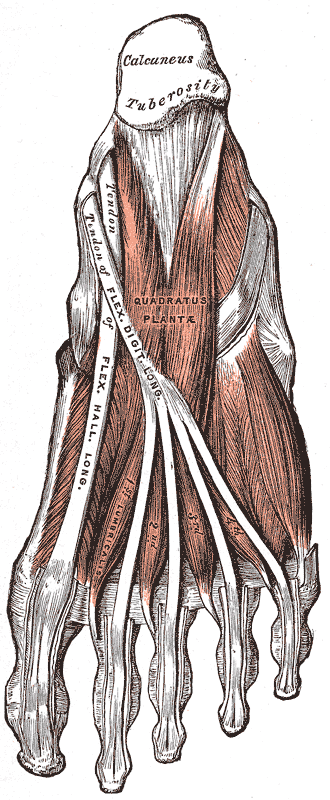
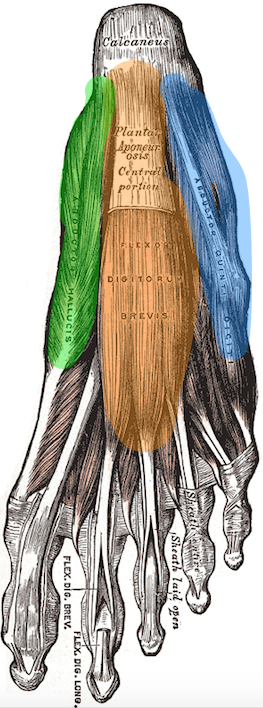
The plantar fascia, just like all the structures in the foot, is capable of generating pain. However, plantar fasciitis is rarely the main diagnosis as the foot is much more complicated than just the plantar fascia. There are multiple layers of muscles and tendons in your feet that are deep in the plantar fascia. See the pictures below.
In addition, muscles originating in your calf will travel behind your ankle and attach onto your foot as well. The picture below (highlighted in blue, green, and yellow) shows the muscles that originate deep in your calf that travel and attach onto the bottom of your foot (depicted as the red shaded areas)
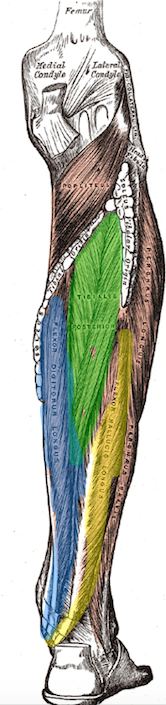
It is clear that there are many structures in your foot and calf that can contribute to pain. All structures in your foot and calf play a role in stabilizing and keeping your foot pain free. Additionally, they are all capable of developing pathology and generating pain.
The most common pathologies that develop in the foot are:
- Adhesion
- Tendon degeneration
Adhesion
Adhesion can form in any muscle in your foot and calf and form from overuse (standing, walking, running). It acts like glue in your muscles causing them to become weak and less flexible. This will generate pain and cause the tendons in your heel to become overloaded and degenerated (more on this below). A soft tissue specialist will break down adhesion with Manual Adhesion Release™ or Instrument Adhesion Release™. Which treatment they will use will depend on the muscles involved. Below are 2 brief video clips of Dr. Phipps utilizing both techniques on muscles that will contribute to your foot pain.
Treatments such as. injections, rolling your foot on a ball, stretching, ice, and anti-inflammatories will not break down adhesion. With expert treatment, this will improve the function of your foot immediately.
Degenerated Tendons.
A tendon is a soft tissue structure that attaches a muscle to a bone. Below shaded in orange, green, and blue are 3 muscles that have their tendons attach onto the heel. These tendons are capable of degenerating and causing heel pain commonly misdiagnosed as plantar fasciitis.
If you have heel pain that occurs when you take the first few steps out of bed or a chair, this is likely one of your diagnoses. The tendons in your feet can degenerate for months or even years without your knowledge, causing it to one day cross a threshold, resulting in pain that doesn’t go away. This degeneration can occur when the load placed on the tendons is too high and the tendon can’t recover properly, causing it to break down and degenerate. Muscle Adhesion and prolonged standing/walking/running are a few sources that create high loads on your tendons.
Firstly, for treatment of degenerated tendons you should have the adhesion treated to decrease the load on the tendon immediately. Load management advice, orthotics and rehab exercise will depend on your personal case. Then properly managing your case and receiving the correct treatment will allow the tendon to regenerate and become healthy again- meaning your foot will be pain free and stay that way.
Contact Phipps Soft Tissue and Spine today to receive the correct diagnosis for your foot pain. Ignoring your foot pain or relying on ineffective treatment methods will only make your condition worse and harder to resolve.
GET RELIEF NOW
To schedule an appointment, please call us at (716) 629-3100 or take advantage of our convenient online form
*Please note that every patient is different. The content and tips displayed on this page are for educational purposes only, and do not substitute for medical advice. Please consult with a medical or healthcare provider, such as Dr. Phipps, for specific diagnosis and treatment advice. Williamsville, NY 14221 Chiropractor
Carpal Tunnel
Carpal tunnel symptoms can come out of nowhere and become a huge intrusion into your life. Researching a symptom you’re experiencing can be helpful to determine where to start. Then, the next step is receiving a proper diagnosis and treatment. However, this can be difficult with the conflicting information available on the internet. In addition, misdiagnosis of carpal tunnel happens often. So getting a correct diagnosis is key before receiving treatment.
This 4 part series will give you the basics regarding tingling, numbness, and pain traveling into the fingers so that you can receive the proper treatment from the correct doctor.
Set up a consultation with Dr. Phipps to get help today!
*Please note that every patient is different. The content and tips displayed on this page are for educational purposes only, and do not substitute for medical advice. Please consult with a medical or healthcare provider, such as Dr. Phipps, for specific diagnosis and treatment advice. Williamsville, NY 14221 Chiropractor
Active Release Technique (ART®)
Active Release Technique is a patented, state-of-the-art soft tissue movement system that has been developed, refined, and patented by P. Michael Leahy, DC, CCSP. It’s the proven method for the breakdown of scar tissue and has become the gold standard in soft tissue treatment. Used by millions of professional athletes, celebrities, weekend warriors, and desk jockeys to stay pain-free.
How it works:
Locate the scar tissue using hands
Make contact with the scar tissue
Brings a muscle through its maximum ROM
Breaking the adhesion down to be absorbed by the body
This will free up the muscle allowing it to perform its job properly
Leading to pain relief
ART can help treat:
Muscles, tendons, ligaments, fascia, and nerves
Headaches
Back Pain
Carpal tunnel syndrome
Shin splints
Shoulder pain
Sciatica
Plantar fasciitis
Knee problems
Tennis elbow
and many others…
*Please note that every patient is different. The content and tips displayed on this page are for educational purposes only, and do not substitute for medical advice. Please consult with a medical or healthcare provider, such as Dr. Phipps, for specific diagnosis and treatment advice. Williamsville, NY 14221 Chiropractor
5 Tips to Maintaining Muscle Health
Most of us perform preventative daily rituals to maintain our health. We brush and floss to prevent cavities and gingivitis. We manage our diet to avoid diabetes and high cholesterol. We take vitamin D during the winter to prevent a deficiency. But what are we doing for our muscles? Taking care of our muscles is important to prevent degeneration of joints and pain. Ultimately we want to wake up in the morning without pain and do the things we enjoy pain in life for as long as possible. Here are 5 tips to help you toward that goal.
TIP #1: LISTEN TO YOUR BODY AND DON’T ABUSE IT.
We commonly abuse our body to the point where we have to either stop doing the activity or take pain medicine to get through the day. Pain is our body’s defense mechanism and warning system that something is being damaged or is already damaged. Think of it as your check engine light. Reducing or removing the pain without fixing the problem, which pain medicine is designed to do, will only cause further damage and pain. It’s like turning off your check engine light without fixing the problem. Short-term relief results in long term chronic problems. It would be like your check engine light coming on because your car oil level is low. You can choose to have the problem diagnosed and fixed for a few hundred dollars or you can ignore it and wait until your engine blows up and you are paying thousands of dollars for a new engine. You only have one shot with your body and listening to it will go a long way.
TIP #2: VARY YOUR ACTIVITIES
Doing the same thing over and over again only results in overuse injuries. Vary your activities and exercises as much as possible to evenly distribute the load over multiple areas of your body. Repetitive activities results in overuse injuries because the same muscles are continuously working.
TIP #3: VARY YOUR INTENSITY
Exercise doesn’t mean going 100% all the time. It is important to have complete rest days and days where you only go 80, 50 or even 30 percent.
TIP #4: FOAM ROLLING, STRETCHING, AND MOBILITY WORK.
Foam rolling, gentle stretching, and general mobility are great for warming up and increasing blood flow to your muscles.
TIP #5: TREAT YOURSELF TO A MASSAGE.
Massage is a great way to increase blood flow to muscles. It also helps with recovery and relaxation.
These 5 tips are like brushing your teeth for your muscles. However they are only useful if you don’t have pain. If you have pain in a tooth, brushing and flossing will not make it go away. Instead you visit your dentist so they can figure out why your tooth hurts. If you have muscle or joint pain, you shouldn’t foam roll and stretch. The first step is getting the appropriate diagnosis and treatment. If you are experiencing pain, call Phipps Soft Tissue and Spine. We will take the time to diagnosis your problem and provide you with the appropriate treatment. Time is not on your side when it comes to pain. Continuing to ignore/cover up the pain can result in permanent damage like tearing and degeneration.
*Please note that every patient is different. The content and tips displayed on this page are for educational purposes only, and do not substitute for medical advice. Please consult with a medical or healthcare provider, such as Dr. Phipps, for specific diagnosis and treatment advice. Williamsville, NY 14221 Chiropractor
Is Swimming Low-Impact?
If you have back pain or a history of back pain, which sport listed below is the least likely to cause more damage?
- Baseball
- Kendo
- Running
- Soccer
- Swimming
Swimming seems like the obvious answer, since that is usually the go-to sport for people with pain. Surprisingly, a recent research article didn’t find this to be the case (1).
Researchers used MRIs to image the lower backs of 306 well-trained university athletes and compared them to 71 non-athlete university students and found that swimmers and baseball players had the highest amount of low back degeneration (1).
With baseball players, it makes sense because of the forces that are involved with swinging a bat. But how does swimming cause so much degeneration? (The rest of this article is a hypothesis on why an increase in degeneration occurs in swimmers.)
Kicking during swimming is a very large part of propulsion. The main muscle that fires during kicking movements is the psoas major (hip flexor). Looking at the green highlighted portion of the picture below, you can see that it attaches to the side/front of the lumbar spine (lower back) and travels down to attach to the femur (upper leg bone).
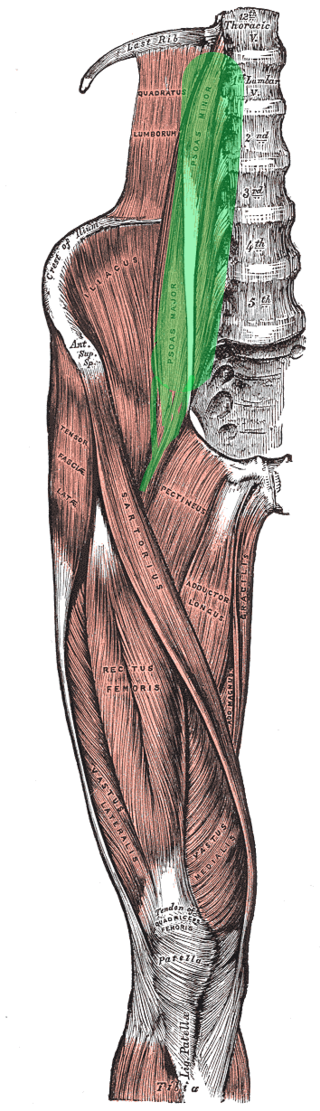
Every time you kick your leg, the psoas contracts, pulling on your low back. This causes the muscles in the back of your lumbar spine to contract to counteract the pulling force from the psoas. The end result is stabilization of your low back. This happens everywhere throughout your body. When one muscle contracts, other muscles contract to stabilize the area and prevent motion. In this case, the repetitive contraction to stabilize your spine during kicking causes increased compression on your lower back discs. The end result is increased disk degeneration.
This doesn’t mean swimming is a bad thing, but it is something to take into consideration. If you have back pain or have a history of back pain, then you may want to reconsider the structure of your swimming workouts. Many workouts will include kickboard drills or kicking with fins (fins will increase the strength of the psoas contraction, leading to more disc compression). These drills will greatly increase stress on your low back. If you know you have degeneration in your low back and still want to swim, it may be a good idea to limit kicking or use a pull buoy to avoid any extra kicking stress. In addition, many people will turn to swimming when they have back pain because it is the only physical activity they can do with minimal pain. I would strongly advise against this because it may only prolong the length of time that you are in pain. It is important to note that if you are experiencing pain, then you should be properly evaluated to determine the cause.
Muscle adhesion is the most common source of pain and stiffness and the most underdiagnosed. If you are experiencing pain or stiffness, please click the button below.
1) Hangai M, Kaneoka K, Hinotsu S, et al. Lumbar intervertebral disk degeneration in athletes. Am J Sports Med 2009; 37:149-155.
*Please note that every patient is different. The content and tips displayed on this page are for educational purposes only, and do not substitute for medical advice. Please consult with a medical or healthcare provider, such as Dr. Phipps, for specific diagnosis and treatment advice. Williamsville, NY 14221 Chiropractor
Stretching: The Solution to Muscle Pain…or is it?
Do you have tight, stiff, or painful muscles? You obviously need to stretch more, right?
If something is tight, stiff or painful, we immediately assume it needs to be stretched. Stretching may provide temporary relief for some, but the majority of people do not get results. Unfortunately, stretching is not the answer to all of your problems. In this article, we will talk about two of the major contributors to your tight, stiff, and painful muscles.
The first contributor is protective tension. Protective tension is the spasm of a muscle to protect an irritated or damaged area. The easiest way to visualize this is to think about someone who has lower back pain. They try to touch their toes but immediately feel their back and hamstrings stretch, which prevents them from bending forward. This is your body’s way of preventing you from loading the irritated and damaged area. Your hamstrings aren’t “tight”; rather, they are contracting to prevent you from causing more damage. Stretching in this case would only make it worse.
The second contributor is adhesion. Adhesions form in muscles mainly from overuse and prolonged positions (sitting and standing). Adhesions are like glue in your muscles that don’t allow them to stretch properly. This leads to tight, stiff, and painful areas because the joint isn’t allowed to move properly. The great thing about adhesion is that it is reversible and, once removed, the muscles and joints can move properly, effectively reducing your symptoms. Adhesions are treated by specific soft tissue work by a certified provider.
The next time something is tight, stiff, or painful, don’t waste your time with stretching. Have it properly diagnosed and treated by a professional. This could save you many problems down the road.
If you have tight, stiff, or painful muscles, please click the button below. Dr. Phipps is a soft tissue specialist located in the Buffalo/Western NY area.
*Please note that every patient is different. The content and tips displayed on this page are for educational purposes only, and do not substitute for medical advice. Please consult with a medical or healthcare provider, such as Dr. Phipps, for specific diagnosis and treatment advice. Williamsville, NY 14221 Chiropractor
Top 4 Foam Rolling Mistakes
1. Only foam rolling AFTER exercise.
Foam rolling is a great way to warm up your body BEFORE exercise. Foam rolling followed by a quick dynamic warm-up is a great way to prepare your body for movement. To learn how to foam roll and perform a dynamic warm-up click the following link: The 6 Characteristics of a Good Dynamic Warm-up by Eric Cressey.
2. Rolling over the greater trochanter.
The greater trochanter is a bony prominence of the femur. If you google it, you can see pictures of it. If you run your hand down the side of your thigh, you will feel a bony bump at the top. When you are rolling the side of your leg avoid rolling over that bump. It can irritate the bursa that is over top of it.
3. Using the foam roller on every muscle.
The foam roller works great for most muscles but it doesn’t work that great in the calf area. Try using a massage stick (The stick) instead. Make sure the calf is relaxed in order to get the deep calf muscles as well. Sit down lifting your knee straight toward the ceiling let your foot relax so it points toward the floor and relax as much as possible as you roll/massage your leg.
4. Using the foam roller to treat pain.
Foam rolling shouldn’t be used to treat pain. Foam rolling may reduce or eliminate your pain temporarily but ultimately it only delays you from getting the proper treatment. Proper treatment involves removing adhesion, which the foam roller cannot do. To learn more about this topic click the following link: Can foam rolling remove adhesion?
If you are experiencing pain or have any questions regarding your pain, please click the button below.
*Please note that every patient is different. The content and tips displayed on this page are for educational purposes only, and do not substitute for medical advice. Please consult with a medical or healthcare provider, such as Dr. Phipps, for specific diagnosis and treatment advice. Williamsville, NY 14221 Chiropractor

